The most helpful Type 1 diabetes care tips we’ve learned so far
 By Jesse Jost
By Jesse Jost
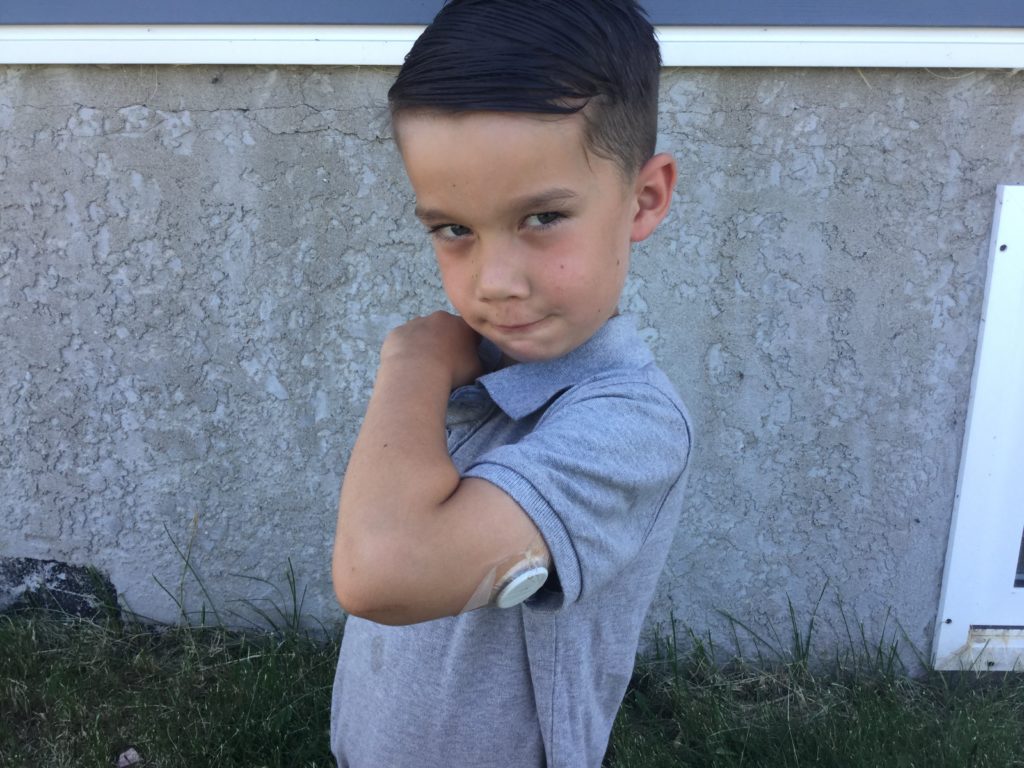
Our world was turned upside down last August when our 5 year old son Elijah almost died from undiagnosed Type 1 Diabetes. Diabetes care involves a huge learning curve. At first the emotions are so overwhelming it’s hard to focus on even the basics. But gradually you can think again and try to sort through the mountain of information. This is a list of tips and info that has really been helpful to us in this first part of the journey. We’re only 11 months in so I’m not sharing this because I think we’re experts – diabetes does a good job of making sure that never happens! I only share because our experience might be useful to someone else.
Of course, diabetes is different for everyone, so trust the advice of your endocrinologist.
The Law of Small Numbers
With diabetes you constantly walk between two dangers: the life-threatening low, and the miserably dangerous high. You have one factor that plummets your blood glucose (BG) – Insulin. And one that rockets your BG : Carbs. The goal is keeping them in balance.
The challenge is all the guesswork: Not always knowing how many carbs are in the food, what the body’s current insulin ratio is, how much the carbs will be burned off by exercise or blocked due to illness.
With so many error factors that multiply exponentially as you increase the carbs or dose of insulin, it makes sense to us to try to keep the carbs and insulin numbers as low as possible. The greater the error in calculation the greater the risk of a stubborn low, or a health-threatening high.
Whenever possible we try to keep carbs at minimum without sacrificing good flavour and eating enjoyment. Saying no to sugary treats is difficult sometimes (understatement alert! It tears your heart out to have to say no to your little guy!) But we try to remember that being high or having sugars drop like a rock would be even more unfair to Elijah. Stable BG is true quality of life.
Low carb is not the only way, however. Many families are wizards with insulin, and have figured out how to achieve stable sugars without a change in diet. Find what works for you.
Push insulin when sick
When sickness comes the appetite usually disappears. It would be easy to think that this is an opportunity to maybe skip a shot of insulin since there is no desire for carbs. However, insulin becomes even more important when ill. Sickness creates ketones, plus the stress of an illness causes the liver to release sugars, which causes BG to rise (regardless of the carbs eaten). High blood sugar and large ketones when mixed turn the blood into an acidic poison and cause a life threatening condition called Diabetic ketoacidosis (DKA)
A non-T1D body will release extra insulin to deal with the extra ketones and BG. But without natural insulin the sick diabetic is at a higher risk of (DKA). Sick days are complicated, but the most important things to remember are: frequent checks of BG and ketones, regular insulin to flush the ketones, even if you have to give juice or popsicles to match insulin dose, and above all, as much liquid as you can drink. If large ketones are present, contact your diabetes team immediately, because DKA can happen quickly the larger the ketones are, and DKA cannot be treated at home.
Stay hydrated
Hydration is a good idea for everyone, but for diabetics, it’s a must. Here’s why:
The body tries to deal with high blood sugar through urination so high BG is a dehydration risk.
Insufficient insulin also allows ketones to accumulate in the body. The body needs to be well hydrated to flush the ketones.
The body’s fluids transport insulin through the body. Dehydration, made worse from high BG, is what makes DKA so serious outside the hospital. When dehydrated, it won’t matter if insulin is injected if there is not enough bodily fluid to transport it. The only solution at this point is an IV. So make sure your diabetic drinks every chance he gets, both as a precaution and to deal with any risks that may be developing.
Avoid the moderate lows as much as possible
Extreme low BG brings the risk of coma, seizures, and brain damage. Thankfully before the diabetic reaches this point, low or dropping BG levels should set off the body’s alarm system and release hormones like adrenaline that will cause the liver to release some life-saving sugar. However, the more frequent the low, the more the body will ignore them. When a diabetic no longer feels his lows, he is in serious danger. Extra care should be taken to avoid lows, not just for the immediate danger of that particular low, but because you want the body to stay alert to lows so that the emergency systems will kick in.
Never Assume. Diabetes is always unpredictable.
Incorrect SWAG-ging (carb estimating), and changing insulin sensitivity make predicting BG difficult enough. But even more maddening is the fact that there are dozens of factors that affect BG apart from what and when you eat: hormones, activity, emotions, illness, ineffective insulin, and many other things make it difficult to know with confidence the direction BG will take. Our random checks have shown results that were completely unexpected and could have been dangerous if not detected. There is no substitute for frequent checks, made much easier by today’s technology of continuous- and flash-glucose monitors.
Show grace!
Diabetes care, either of yourself or a loved one, exacts a huge emotional toll. It frazzles nerves and robs sleep. The stakes of whether or not you achieve stable sugars are so high that there can tremendous pressure to achieve a share-worthy graph. But diabetes doesn’t play fair and often throws you a two-ton curveball, causing the BG line to look a silhouette of the Rocky Mountains. When this happens, there can be the crushing weight of guilt combined with fears of the damage these erratic numbers are doing to the body. You can’t beat yourself up. There is far too much out of your control.
Numbers are not report cards of failure. They are simply information that is enabling you to give better health. Show grace to yourself and your spouse or partner. Make it a habit to never criticize. Constantly making dosing decisions on wildly unreliable or incomplete data is exhausting. When hindsight shows that you gave too much insulin, or too many carbs, it’s not your fault! You are doing the best you can and BGs just as easily could have gone the other way. Don’t preen when it goes right and don’t wallow when it goes wrong. It just as easily could have gone the other way. Show affirmation to the T1D caretakers in your life. They need it!
Try to be thankful.
It’s so easy to start being overwhelmed with grief or self-pity for all the inconveniences diabetes causes. It’s okay, there is a time for grief and tears are a gift. There will be many times you just need to vent. But in between, try to hang onto the positive. We speak this from the trenches, and know how hard it can be to do! You’re dealing with enough challenges that take your energy… don’t get drained by discouragement, too. It’s a true wonder that today Type 1 diabetics can thrive and enjoy a high quality of life thanks to modern insulin and BG monitors.
For most of history, diabetes was a death sentence; a starvation diet was the closest thing to a cure. Even after the discovery of insulin, the insulin, when available, was often inconsistent, dirty, and the needles were painful and caused abscesses. The only ways to know your BG level was a to give a huge blood sample at the hospital and wait for days. Or mix your urine in a solution overnight and see what color it turned. By that time the information was too old to be really useful. Today we have clean, reliable insulin, almost painless needles, pumps and dexcoms. All these extra gadgets and supplies we have to carry are truly miraculous gifts that other people would have paid a fortune for. Remembering this might just make that painful shot a little easier to give.
